 | . | Step 30 of 41 |
 |
Clinical Stem 1
Non-smoking female with a new right upper lobe lung mass and three PET-positive mediastinal lymph nodes
Non-smoking female with a new right upper lobe lung mass and three PET-positive mediastinal lymph nodes
Answer D
On the other hand, for cytological diagnosis, the diagnostic yield of bronchial brushings in central lesions is 59% compared with approximately 46% for peripheral lesions. The utility for molecular markers analysis has not been clearly determined.
Bronchioloalveolar lavage has a diagnostic yield of 48% for central lesions and 43% for peripheral lesions. There is emerging data on the use of lavage for molecular analysis but a major limitation relates to tumor cellularity.
EBUS-TBNA from abnormal mediastinal/hilar nodes in patients with known or highly suspected lung cancer has a diagnostic yield for malignancy of 94% with usually at least 3 specimens per nodal station being obtained for diagnosis if ROSE is not utilized. Two aspirations per nodal station are considered acceptable when at least one core is obtained from the first two specimens. For molecular markers, adequacy of EBUS-TBNA specimens varies in the published literature between 72-99%.
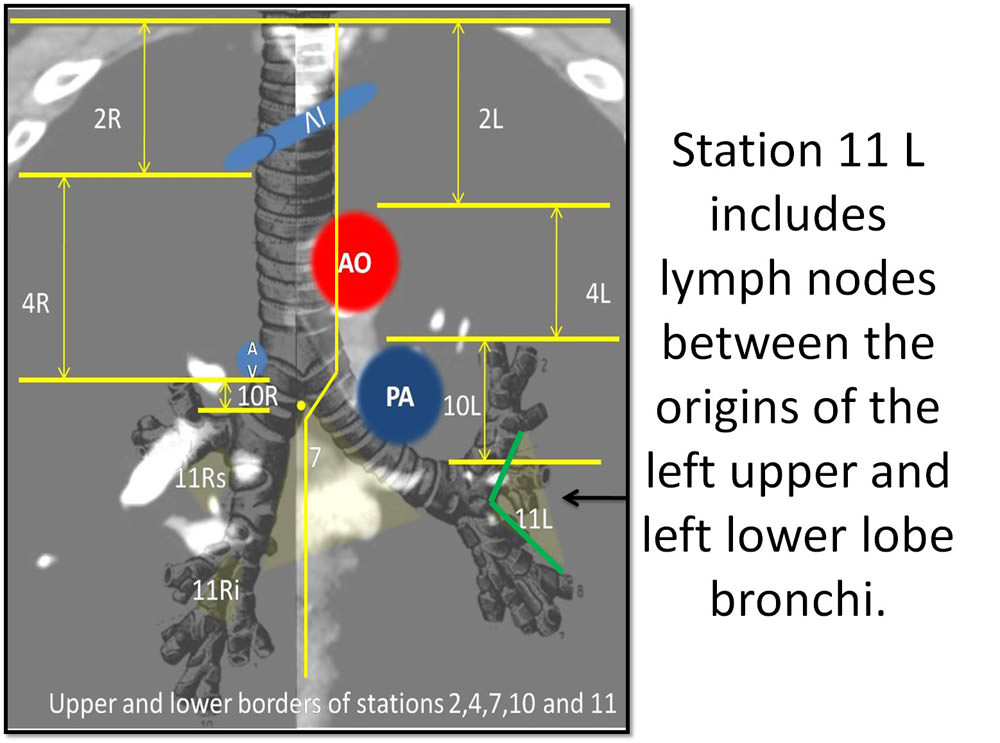
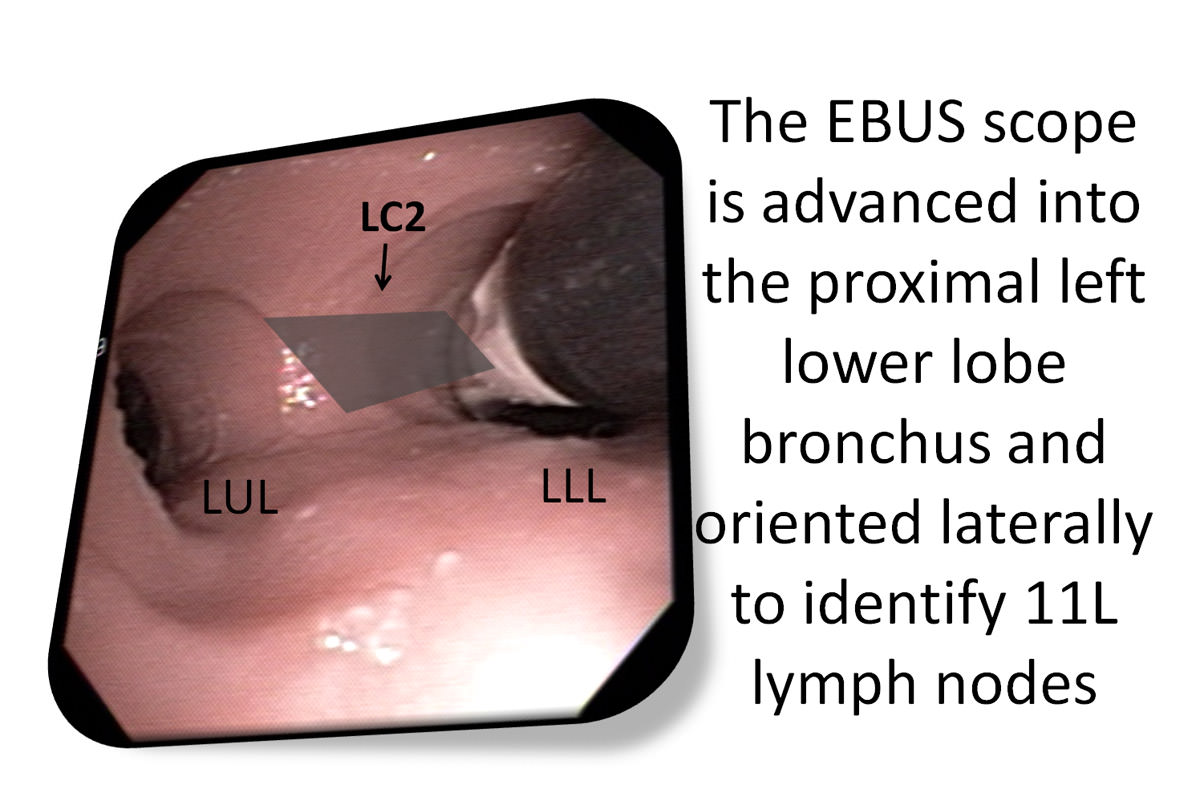
In this patient, combined sampling techniques are warranted. Using EBUS-guided TBNA, left-sided nodes should be sampled first since the patient's primary tumor was on the right. A reasonable approach, therefore, would be to start with the newly PET-positive 11L node followed by sampling nodes at level 4L and potentially 4R.
Published literature supports a practice of combined techniques to increase the yield for central lesions for which the diagnostic yield is 88% versus 69% for peripheral lesions. Brushing and washing increases diagnostic yield by up to 17%.
The utility of bronchoscopic specimens for molecular marker analysis is based on the number of intact malignant cells provided for analysis. Because of this, specimens with malignant cells in suspension can be prepared in cell block for immunohistochemistry or submitted for molecular testing, a combination of endobronchial techniques and EBUS-TBNA techniques seems to be the most advantageous in terms of specimen acquisition for molecular analysis.
References:The utility of bronchoscopic specimens for molecular marker analysis is based on the number of intact malignant cells provided for analysis. Because of this, specimens with malignant cells in suspension can be prepared in cell block for immunohistochemistry or submitted for molecular testing, a combination of endobronchial techniques and EBUS-TBNA techniques seems to be the most advantageous in terms of specimen acquisition for molecular analysis.
- British Thoracic Society guidelines on diagnostic flexible bronchoscopy Thorax 2001;56:(suppl I) i1?i21.
- Arcilla M, et al. Rebiopsy of Lung Cancer Patients with Acquired Resistance to EGFR Inhibitors and Enhanced Detection of the T790M Mutation Using a Locked Nucleic Acid-Based Assay Clin Cancer Res 2011;17:1169-1180.
- Van der Drift M, et al. The Additional Value of the Ras-Association Domain Family 1A Gene Methylation and Kirsten Rat Sarcoma 2 Viral Oncogene Homolog Mutation Analyses in Washings in Nondiagnostic Bronchoscopy Chest 2012;141;169-175
- Tanner NT, et al. Utilizing Endobronchial Ultrasound With Fine-Needle Aspiration to Obtain Tissue for Molecular Analysis J Bronchol Intervent Pulmonol 2011;18:317-321.







