 | . | Step 39 of 40 |
 |
Clinical Stem 2
A patient with pulmonary nodules 1 year after curative intent resection of primary lung adenocarcinoma
A patient with pulmonary nodules 1 year after curative intent resection of primary lung adenocarcinoma
Answer E
Repeat thoracentesis is not warranted because of the rapid recurrence of the effusion and a likelihood this patient will live more than one month if her effusion and symptoms are controlled by other minimally invasive procedures
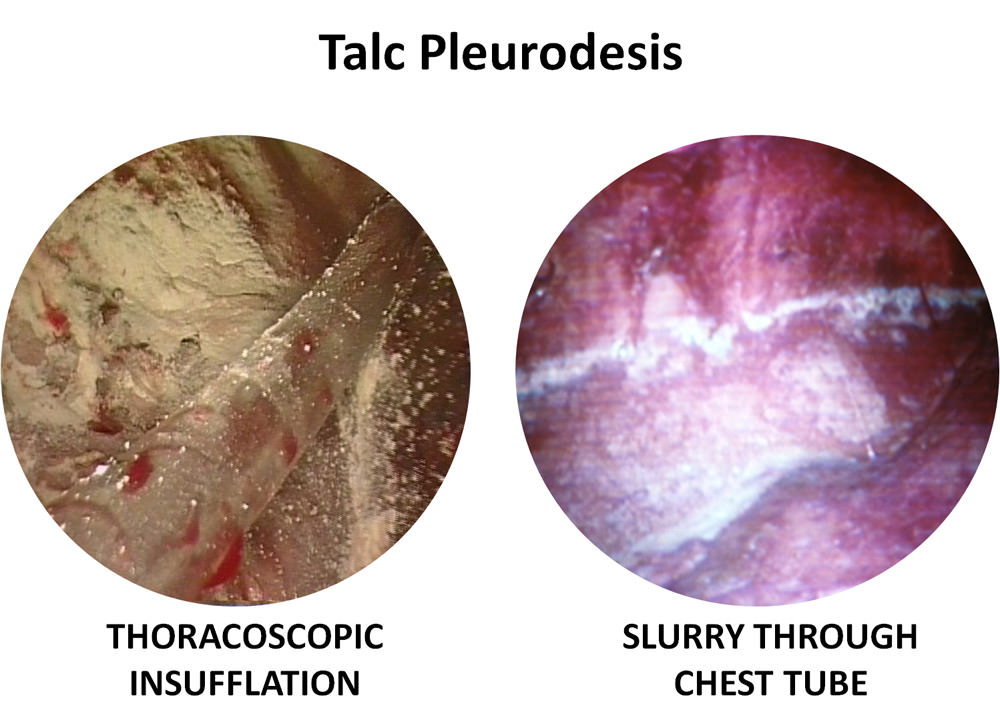
Rigid thoracoscopic or pleuroscopic talc insufflation pleurodesis is better than talc slurry, especially in patients with malignant effusions from lung and breast cancer. Respiratory complications including respiratory failure have been reported after insufflation and slurry.
Results from clinical trials show that tunneled pleural catheters, also known as TPCs, result in reduced post-procedure and overall length of stay compared with thoracoscopic talc insufflation or chest tube talc slurry pleurodesis. There are no differences in complication rates or in-hospital mortality. TPC placement may also be associated with significantly fewer ipsilateral re-interventions. TPCs are somewhat superior to talc slurry in terms of reliable drainage, pleurodesis and survival with effusion control but there may be no significant differences in quality of life between the two strategies.

Lung cancer patient management decisions take into account the patient's values, overall state of health, need for hospitalization, performance status, desire to return home, indications for hospice care, and physician biases, preferences, experience and degrees of expertise as well as the patient's ability and informed consent to undergo minimally invasive procedures under local or general anesthesia.
References:- Hunt BM, Farivar AS, Vallieres E, et al. Thoracoscopic talc versus tunneled pleural catheters for palliation of malignant pleural effusions. Ann Thorac Surg. 2012;94:1053-7.
- Fysh ET, Waterer GW, Kendall PA, et al. Indwelling pleural catheters reduce inpatient days over pleurodesis for malignant pleural effusion. Chest. 2012;142:394-400.
- Demmy TL, Gu L, Burkhalter JE, et al.Cancer and Leukemia Group B. Optimal management of malignant pleural effusions (results of CALGB 30102). J Natl Compr Canc Netw. 2012;10:975-82.
- Davies HE, Mishra EK, Kahan BC, et al. Effect of an indwelling pleural catheter vs chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion: the TIME2 randomized controlled trial. JAMA. 2012;307:2383-9.
- Dresler CM, Olak J, Herndon JE 2nd, et al. Cooperative Groups Cancer and Leukemia Group B; Eastern Cooperative Oncology Group; North Central Cooperative Oncology Group; Radiation Therapy Oncology Group. Phase III intergroup study of talc poudrage vs talc slurry sclerosis for malignant pleural effusion. Chest. 2005; 127: 909-15.
- Stefani A, Natali P, Casali C, et al. Talc poudrage versus talc slurry in the treatment of malignant pleural effusion. A prospective comparative study. Eur J Cardiothorac Surg. 2006; 30: 827-32.







